Case history-7
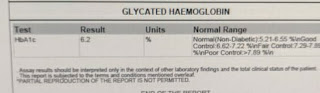
A 12 years old boy, studying 9 standard, from Nalgonda presented to opd 4 days back with cheif complaints of shortness of breathe and orthopnea. History of past history: Patient was apparently asymptotically 2 month back .he developed high grade fever and referred to local hospital Fever was subsided after 2 days.After one month he suffered with vomitings at night . They is no incident of any blood in vomitings. He then immediately went to Hyderabad and found that his urea and creatinine levels are increased . They immediately started dialysis .five sessions of dialysis have been done. Patient suffered with chest pain only during sOB No history of pedal edema,facial puffiness ,no decreased urine output Past history: Hypertensive since 1 month No history of asthma,epilepsy, thyroid disorders Patient was undergone 3 transfusions 1 month back Patient has increased sugar level which is subsided 1 week back Family history: No his...

